The pathology of hemorrhoids
BETTER UNDERSTANDING, BETTER HEALING!
What is a hemorrhoid?
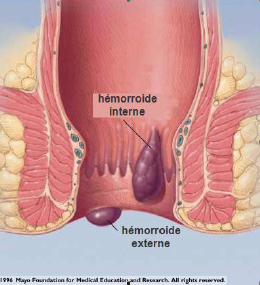
A hemorrhoid is a vein, or rather a venous network, located in the anal canal.
What people commonly refer to as “hemorrhoids” are in fact varicose veins: they are called hemorrhoidal varices, or simply hemorrhoids.
What are some of the frequent causes of hemorrhoids? There are many, including:
- A family history, either on the mother or the father’s side
- Pregnancy
- Constipation
- Lifting heavy objects
- Reading on the toilet
- Gardening in a crouched position
In short, hemorrhoids are anorectal varicose veins, and anything that increases intra-abdominal pressure can cause hemorrhoidal veins to swell and varicose veins to form.
In particular, some people have developed the habit of staying on the toilet for extended periods of time (10 minutes or more): either they are waiting for a bowel movement, or they like to read in peace. Regardless of why they do it, it’s a sure way to develop hemorrhoidal varicose veins!
What should you do then? If you are unable to defecate, don’t wait more than three minutes. Get up and do something else. The urge to defecate will return and you will be able to complete the task. This enables the individual to remain in control of his/her rectum instead of the other way around.
 Grading of hemorrhoids
Grading of hemorrhoids
Surgeons grade hemorrhoids according to the following scale:
- Grade 1: No prolapsus. Hemorrhoids remain inside the body. If there are no symptoms such as bleeding or discomfort, they can be left untouched.
- Grade 2: Spontaneously reducible prolapse. This occurs when hemorrhoids protract and retract on their own. In this case, they can easily be ligated.
- Grade 3: Prolapse with manual reduction. Hemorrhoids must be manually pushed in. Hemorrhoids such as these can be ligated.
- Grade 4: Non-reducible prolapse. Hemorrhoids that do not retract even with pushing. Such hemorrhoids may require a different therapeutic approach, cryotherapy or even surgery.
A combination of several grades is often observed in the same person.
Recurrence of hemorrhoids after treatment in clinic
Hemorrhoids can recur after ligation treatment on the internal hemorrhoid. We try to decrease the rate of recurrence by adding cryotherapy treatment to the external hemorrhoid.
What are the common causes of recurrence? They are all related to the sustained increase in venous pressure in the pelvic region and especially in the hemorrhoidal veins.
Pregnancy is therefore a common cause.
The frequent lifting of heavy objects.
Straining to defecate in the event of constipation.
However, the most frequent cause is prolonged crouching:
- Staying on the toilet for prolonged periods, generally while on the phone or reading
- Prolonged crouching related to:
- work (electrician, painter, plasterer)
- leisure (gardening, yoga, gym)
- sports (weightlifting, mountain biking, skidooing, baseball)
Regular squats are not a problem since they do not require remaining in a squatted position for a prolonged period.
The problem can be somewhat alleviated by:
- resolving constipation issues
- using knee pads or a small bench while gardening
The amount of time spent on the toilet is, by far, the most frequent cause and is definitely a habit worth breaking.
Generally speaking, you shouldn’t spend more than two or three minutes sitting on the toilet. This is more than enough time to empty the rectal ampulla.
If it feels as though you have not finished defecating, it means that there is a fecal bolus in the sigmoid colon. In this case, it is best to get up and do something else while waiting for the urge to defecate to return a bit later (often a few minutes later). This second period of two to three minutes is usually enough time to complete the task.
Sometimes people stay on the toilet for extended periods because they need some time alone.
However, spending 15 or 30 minutes, and in some cases even more time, in this position increases venous pressure on the hemorrhoidal plexus, which causes new hemorrhoidal varicose veins to form.

For a visit concerning hemorrhoidal issues
Preparing for the visit
It is advisable to take an analgesic (Tylenol or Advil, if there is no contraindication from your family doctor) one hour before your visit, as you will probably be getting rubber band ligation and cryotherapy treatment. Although the treatment itself is generally quite tolerable, there may be some discomfort and sometimes even pain, usually of short duration (15 to 30 minutes).
It is important to stop any blood-thinning medications (that prevent clots from forming) to help ensure that you do not experience significant bleeding following the procedure. These may include anti-platelet drugs (Aspirin, Clopidogrel (Plavix) or others) or blood thinners (Coumadin, Eliquis, Xarelto or others). Most of these medications should be stopped the morning of the procedure and for at least 7 days afterwards. It is important to get your doctor’s approval before stopping any of these medications.
What to expect during the procedure
Although likely to cause a great deal of apprehension, this examination and the ensuing treatment procedures usually go very smoothly. Your doctor will explain each step. After asking a few questions, he or she will begin by inspecting the anal area and then perform a finger examination (digital rectal exam). He will then insert a small scope through the anus to view the internal hemorrhoids. Once he confirms the presence of hemorrhoids, he will proceed with the treatment after obtaining your approval. The treatment will consist of rubber band ligation followed by cryotherapy. The whole procedure lasts only a few minutes and, although uncomfortable, is generally not very painful.
Internal hemorrhoids are usually treated at a rate of one hemorrhoid per visit to ensure proper visualization and to avoid complications.
What to expect after the visit
Immediately following the procedure, you may feel an urge to defecate. This is almost always a false urge that will disappear spontaneously within one (or a few) hours. It is not dangerous to have a bowel movement after the procedure, but if the bowel movement does not come easily, you should avoid any straining and understand that it is probably just a false urge.
On occasion, patients may experience some pain following the procedure. This varies from one time to the next, so patients may likely experience either more or less discomfort than they did during a previous procedure. This pain is usually moderate and relieved by painkillers (Tylenol or Advil) or anti-inflammatory drugs (Aleve or Naproxen). Sitz baths (sitting with your buttocks in warm water) can also help. Finally, make sure you keep your stools soft by getting enough fibre and water or taking laxatives available by prescription or over-the counter on the advice of your pharmacist.
In the days following the ligation, the hemorrhoidal varicose veins becomes necrotic and combines with the stool. The elastics are released (2 to 10 days) and are evacuated. A wound then forms at the ligation site. This wound may bleed slightly, especially if the stool is rough. A little blood may be seen in the stool or even on the toilet paper, and more rarely in the toilet water. The amount of blood is minimal and bleeding usually stops within two or three days.
The wound then heals and, at the subsequent visit, a whitish scar can often be seen at the ligation site.
When should you worry?
If very heavy bleeding (such as hemorrhaging) occurs, then an emergency room visit is required. This is rare and usually associated with the use of anticoagulants.
If the pain is very severe, and not relieved by medication, if it is accompanied by fever or an inability to urinate, it is important to consult a doctor.
In these circumstances, you can call the clinic during business hours (7:00 a.m. to 1:00 p.m.) and leave a message. We will return your call. Outside of business hours or days, you will need to go to the emergency room.
How to treat hemorrhoids
Treatment of internal hemorrhoids
First off, it is important to ensure that the symptoms are not caused by another condition. For example, the presence of blood can be the result of an anal fissure, proctitis or a tumor. This is why it is so important to perform a differential diagnosis.
If hemorrhoids are identified as being the cause of the symptoms, the most appropriate treatment is then chosen. Very often, the creams and ointments offered on the market only provide temporary and partial relief. If this is the case, it is time to consult a doctor.
For over 25 years, other treatments have been preferred over surgical treatment in the vast majority of cases. Hemorrhoid surgery has a reputation for being very painful: indeed, patients often have to endure severe pain for anywhere from two to four weeks. Furthermore, surgery does not in any way prevent hemorrhoids from recurring.
Several other techniques have been attempted with a view to replacing surgery and only one has proven to be superior to all other methods: hemorrhoidal ligation.
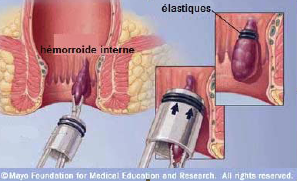
The procedure consists of sucking the hemorrhoidal vein into a small cylinder, then ejecting two elastic bands at the base of the hemorrhoidal varicose veins. This results in strangulation of the vein.
When the technique is performed well, ligation is not painful. The patient experiences discomfort that usually lasts about twelve hours. He will also feel a false urge—in other words, the need to defecate—(even if the rectal ampulla is empty).
The exception is when patients have a concomitant anal fissure. In this case, the pain can be more severe, sometimes lasting up to a week. Patients are generally given analgesic medication or ointments in this particular situation.
After two to three days, the necrotic hemorrhoid and the rubber bands combine with feces.
A little blood can often be seen in the week following the ligation. This occurs when the hemorrhoid falls off.
After one or two weeks, a whitish scar will often appear at the ligation site.
In addition to eliminating the hemorrhoid, the ligation technique creates a small scar that keeps the mucous membrane in place and helps prevent new hemorrhoids from forming.
As most patients generally have two or three hemorrhoidal bundles, the treatment is done over two or three sessions.
In certain cases, more than one ligation can be done during the same visit. This does, however, result in greater discomfort.
When the decision is made to treat more than one, such as when two hemorrhoidal bundles are bleeding, you can expect more pain in the days that follow, but the pain remains moderate in most cases.
Exceptionally, up to six ligations or more can be done in one session, but this is quite rare.
Treatment of external hemorrhoids
External hemorrhoids should not be confused with other lesions that can be found at the anal margin: skin tags, condylomas, tumour lesions or others. It is the physician’s role to determine the nature of the lesions observed.
External hemorrhoids are the result of hemorrhoidal swelling (internal and external) that has occurred in the past, for example during pregnancy. They are strips of skin that usually cause few symptoms.
Their main disadvantage is that they interfere with local hygiene when they are bulky. Their appearance can also be a cause of concern for certain people.
When treatment is prescribed, the lesions can be surgically removed under local anesthesia, although cryotherapy is sometimes sufficient for smaller lesions.
In most cases, it is best to leave them where they are, while ensuring good local hygiene.
Practical advice
Before, during and after your visit to the proctology clinic – For anal surgery


